What is personality disorder (PD)?
Personality of the person is something that defines them. It is the way one thinks and acts in different situations. Personality disorders are a group of disorders in which the personality of the individual interferes with normal functioning or poses problems in relationships.
Overall it has been seen that one in every 10 individuals suffers from a personality disorder. Many individuals with personality disorders also suffer from other psychiatric illnesses and approximately one in every three patients attending psychiatric services has a personality problems.
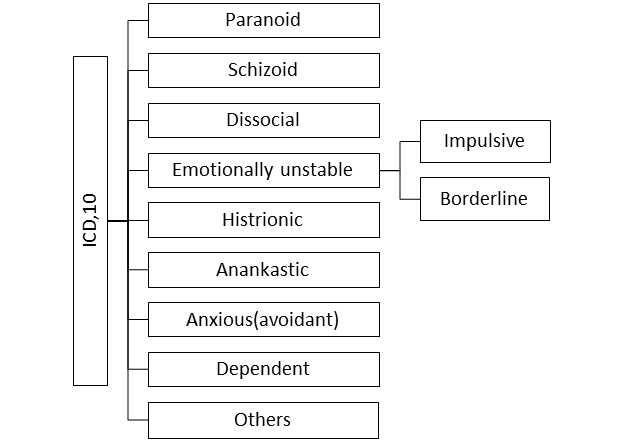
The International Classification of Diseases (ICD) 10th edition by the World Health Organisation classifies personality disorders as follows:
A brief description of each disorder is given below:
-
Paranoid personality: These individuals have marked paranoia due to which they might misinterpret normal actions as hostile. The different spontaneous environmental perceptions may be interpreted with reference to self. These traits lead to trust issues with other and the individual might bear grudges against others. But, unlike patients suffering from schizophrenia they don’t experience fully formed delusions (i.e. their paranoia is less permanent and it may be shaken by presenting the evidence)
-
Schizoid personality: People with schizoid traits prefer to be aloof, indifferent, and detached from others. There are limited activities that interest them, even no desire to have close relations. They may be less sensitive to social norms and mostly don’t think about others. Unlike people with autism, people with schizoid personality have better communication skills and there are no stereotypical (repetitive purposeless) activities noted.
-
Dissocial/Antisocial personality: Usually they are involved in Antisocial activities. There is a lack of concern about others feelings, or social obligation. There are frequent acts of lying, shifting responsibilities and denying responsibilities. Usually there is a history of conduct disorder before the age of 15 years.
-
Emotionally unstable personality: As the name suggests these patients have problem in emotional regulation. A little good news and they are over joyous and a little bad news they feel rejected, sad, alienated, etc. They are further classified into two categories i.e. impulsive type and borderline type
-
Impulsive type is characterised by sudden anger outburst, unstable moods, acting without thinking of the consequences and taking sudden decisions
-
On the other hand, borderline type is characterised by uncertainty about self-image and disturbance in perception of others. In addition to this there may be chronic feeling of emptiness and a fear of being abandoned by others. There might be instances of multiple self-harm attempts or threats.
This is different from complex PTSD as the latter results from experiencing repeated trauma and is a direct result of it.
-
Histrionic personality: There is overexpression of emotional reaction and overconcern with physical attractiveness. They continuously seek attention and excitement so much so that sometimes it may be exceed social limits e.g. inappropriate seductiveness.
-
Anankastic personality: they are described as obsessive, having rigid perfectionism, being extremely careful while doing tasks and excessively sticking to rules and social convention. Thus, there is extreme rigidity in behaviours and undue preoccupation with productivity to an extent that emotional and interpersonal pleasures are ignored.
-
Anxious (avoidant) personality: People with Anxious or Avoidant personality are characterised by persistent apprehensions and worries, low self-image, fear of being criticized. Thus, they live a restricted life and there is avoidance of social, occupational activities, or romantic relationships.
-
Dependent personality: They are dependent on others for making everyday decisions for them. There is an excessive concern about not being able to take care of oneself and their self-confidence is low. Due to this there is less disagreement with others and usually they give in to decisions of others.
-
Other specific personality disorders (eccentric, haltlose, immature, narcissistic, passive-aggressive, and psychoneurotic): Narcissistic personality is more common amongst these. They are characterised by a grandiose feeling and having a notion of holding a special status, in addition the perception is coloured by self-centeredness, and they are usually condescending towards others. Resultantly there are excessive attempts to seek admiration from others.
-
Personality disorder unspecified: includes other personality traits not covered elsewhere
In the upcoming ICD 11 there are proposed changes which aligns it to the recent concept of personality disorders. Two main changes are suggested i.e.
-
The level of severity of dysfunction (i.e., mild, moderate, and severe) should now be evaluated in each case and
-
The diagnosis is now covered under five broader domains i.e. negative affectivity, detachment, dissociality, disinhibition, and anankastia.
How do I know I have personality disorder?
It is common to have certain traits from different personality domains but that does not mean that there is a disorder e.g. a person might have some pervasive anxiety (anxious trait), may seek everyday decisions from others (dependent trait), and be demonstrative in behaviour (histrionic trait) but still be able to function well in all domains of life. These traits may be there from childhood and they may define them. Eventually with increasing responsibilities or demanding situations may push the limits of the person and cause dysfunction. The dysfunction may be in interpersonal, social, or occupational domain which causes significant distress to the individual or the near ones. If help is sought from professionals in time further damage (developing strained relationships, having psychiatric illness, addiction etc.) can be prevented.
What are the causes of personality disorder?
Personality disorder may arise due to one of many reasons. Biological factors like genetics are believed to play some. Usually they are believed to arise from experiences in the early childhood and trauma in the past lead to change in one’s perception and behaviour.
Having cold parents who neglect the needs of the child, lack of protective parents, having sensory disability or being from minority may all lead to paranoid or schizoid personalities.
Borderline, dissocial and histrionic personality results from lack of healthy attachment figures in childhood, or the child may experience conflicts at home, this may result in experiencing trauma in childhood, death of someone near, or frequent migration.
Rejection by parents, isolation in childhood, inconsistent parenting, excessive parental control may lead to anxious, anankastic or dependent personalities.
The factors mentioned above cause a change in the thinking of the individual and eventually the person starts using unconscious defence mechanisms persistently. With time these traits are deeply ingrained as a part of persona and reflect in all behaviour.
Is personality disorder similar to mood disorder?
It is common for patients with different kinds of personality disorder to suffer from co-existing mood disorders, but the two are not the same. While mood changes may be seen in patients with personality disorder, like frequent fluctuations in mood, varying from extreme sadness to extreme happiness, in patients with emotionally unstable personality disorder, or anxious mood particularly in social situations in anxious avoidant personality disorder. They may often be difficult to differentiate from bipolar/ depressive disorder or anxiety disorders.
The difference, however, may be noted in longitudinal observation, where mood changes may show fluctuations or may be seen transiently in personality disorder, while they may remain persistent and pervasive in mood disorders. Furthermore, the mood disorders usually develop in 20s or 30s and have episodic course. After the episode subsides the individual may become well-adjusted and functional.
Personality disorders, on the other hand, have no definite onset as they appear in a mild form early in life, they run a more enduring course and other features apart from mood changes may be apparent to help differentiate them from mood disorders.
The overall the prevalence of having mood disorders is higher among personality disorder clients compared to the general population, and the presence of mood disorders in such individuals indicates a poorer prognosis.
What is the difference between psychosis and personality disorder?
While some personality disorders may be associated with features like feeling suspicious of people and thinking that they are conspiring against oneself (paranoid personality disorder) or fleeting hallucinations or half-formed delusions (schizotypal personality disorder) or extreme agitation and irritability (emotionally unstable personality disorder), these are not the same as psychosis. Such symptoms are either transient, half-formed, and often associated with little conviction.
The risk of eventually developing a psychotic illness may be slightly higher than the general population in certain personality disorders (e.g. schizotypal personality disorder), they themselves do not qualify as being psychotic disorders primarily. Because of these fleeting psychotic symptoms (not amounting to psychotic disorder), low dose antipsychotics are often proven to show some benefit in management of some personality disorders.
Is there a treatment for personality disorder?
There is no absolute treatment for personality disorders as personality is what defines a person. The problem in personality disorders is the maladaptive responses and inability to adapt with different situations which develops over time. Thus, the aim of treatment is not to change the person but to make them more functional and improve their adjustment with society. More than half of the individuals mature out of their Personality Disorder with advancing age as we don’t see many antisocial or borderline patients in the elderly population.
Supportive psychotherapy and crisis management are offered at the time of adverse situations. In some cases e.g. self-harm even short-term hospitalisation is warranted. Usually a long-term therapy is planned aiming at reversal of the maladaptive behavioural patterns which have developed over years.
Different therapies like psychodynamic or Cognitive-behavioural therapy are useful in decreasing these patterns. Some specific therapies like dialectic behavioural therapy in borderline PD patients are based on specific problems of these individuals. Learning interpersonal skills and stress management techniques can also be helpful to them. In a few patients social skills training may be helpful in improving ones adjustment in society. On the other hand family therapy or couple therapy may be offered in case there are issues in family and marriage.
Where should I seek help from?
If you or your dear ones are having symptoms mentioned above with significant distress or problems in carrying normal activities, you should consult your GP or psychiatrist. The psychiatrist will evaluate for symptoms of personality disorder, whether you require treatment or not and order any investigations if required.
The cases where psychiatric admission may be indicated are – if the patient has high suicide risk, is unable to take adequate care of themselves, is a danger to others, needs intensive therapy, or there are medical/psychiatric complication.
Recommended Reading:
- Personality disorder | Royal College of Psychiatrists. Available from: https://www.rcpsych.ac.uk/mental-health/problems-disorders/personality-disorder
