What is psychosis?
Psychosis has been used to describe a situation when a person loses touch with the outer reality. The person may have different symptoms including hallucinations, delusions, or thought disorders.
| International classification of Disorders 10e (ICD-10) define Psychosis as a convenient descriptive term indicating the presence of hallucinations, delusions, or a limited number of severe abnormalities of behaviour, such as gross excitement and overactivity, marked psychomotor retardation, and catatonic behaviour |
Symptoms experienced by patients are:
-
Delusions: These are unusual and unshakable beliefs held by the individual which are believed to be absurd or false by others around them. Beliefs like “The anchor in the TV show is talking about me and giving me signals” or “I can make it rain on my wish”. The patient has full belief in them and holds the belief even when sufficient evidence to the contrary is presented to them.
-
Hallucinations: It is an experience of sensation like sound, smell, taste, vision, touch felt by a person without having any source to cause it e.g. being able to hear someone shouting one’s name despite no one being around.
-
Thought disorder: This involves a problem in constant flow of thoughts or being able to properly organise one’s own thought. Patient may appear to jumble words/sentences or say words without any meaning.
-
Catatonia: In this there is an impaired ability of the patient to move or speak in a normal manner. The patient may appear to be in an uncomfortable postures for a long time or may repeat words or actions repeatedly. However few patient paradoxically may even become excited and agitated.
Not every patient has all the symptoms, but there can be a single or a combination of symptoms in every patient. Usually the patient does not believe that there is anything wrong with them and thus does not acknowledge any unusual behaviour as a symptom.
How do I know I have psychosis?
Majority of patients who have this illness won’t even recognise that something is wrong with them, as they would have lost insight. Due to this there is hesitancy to take any treatment or medication without which the disease might progress and become more difficult to treat eventually. It is therefore best to listen to your well-wishers such as family and friends and the professionals. The patient cannot be the best judge of their situation.
Is having paranoia normal?
Paranoia is a symptom itself and not a diagnosis. If very brief it may be a part of the normal experiences for many individuals. With individuals having Paranoid personality disorder these experiences may be more frequent and involve more than one situations. They have issues with trusting others and are even suspicious at times. These symptoms are usually there since teenage, but this behaviour is neither odd nor bizarre in nature like the experience of patients with schizophrenia. Usually these individuals function well and have problems only when there are extreme situations, or these paranoid ideas interfere with the situation. The main difference between paranoid personality disorder and paranoid psychosis is that psychotic patients suffer with clear cut delusions which are deeply entrenched.
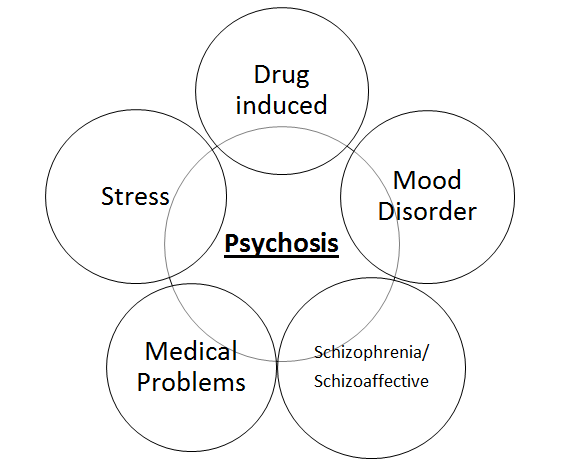
What are the causes of psychosis?
Psychosis may indicate one of the many underlying problems ranging from medical illnesses to Psychiatric disorder. Sometimes it may arise due to underlying trauma like witnessing the death of someone close, which is commonly known as a “psychotic breakdown”. On the other hand it may be a signal of underlying medical issues like stroke, dementia, chemical changes in brain etc. People using recreational drugs such as cannabis or LSD also experience such symptoms. While people suffering from psychiatric disorders like schizophrenia, depression and Bipolar disorder may also report such symptoms.
-
-
Drug induced psychosis: It has been classified in the International classification of diseases – 10 under the under the category of Psychotic Disorder due to Psychoactive Substance use F1x.5 (where “x” varies with type of substance). Psychosis may occur in intoxication phase, or in withdrawal phase.
-
The drugs that may lead to psychosis during acute intoxication are – cannabis, cocaine, LSD, methamphetamine, mescaline, psilocybin, ecstasy, MDMA etc. Withdrawal of certain substances such as alcohol, sedative and hypnotic drugs may also lead to symptoms of psychosis. It may also be seen as an adverse reaction to prescription drugs such as steroids and bupropion, ketamine, drugs used in parkinsonism, etc. If the individual is having pre-existing mental illness then there might be a worsening of symptoms after using these substances.
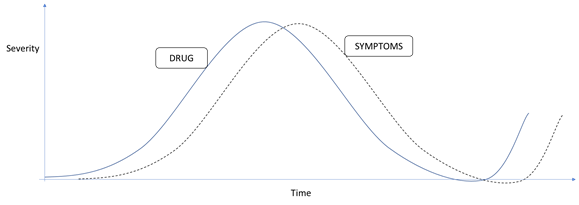
In order to distinguish drug-induced psychosis from schizophrenia experts observe a relation of substance with the symptoms, generally psychosis due to drug use occurs during or immediately after drug use or sudden increase in dose (usually within 48 hours). Similarly it should decrease with a decrease in dose and usually subside after stopping the drug sometimes up to a month of use. These symptoms reappear after reinitiating the substance.
-
 Schizophrenia: Psychotic symptoms are at the core of schizophrenic illness. The distinguishing features of psychosis in a patient suffering from Schizophrenia are that they are chronic, longer lasting, stable (i.e. symptoms don’t change frequently). It may also be that they are more bizarre and associated with incongruent moods, and are more disabling than other type of psychosis. Thus, it is important to rule out other possibilities before making a diagnosis of Schizophrenia.
Schizophrenia: Psychotic symptoms are at the core of schizophrenic illness. The distinguishing features of psychosis in a patient suffering from Schizophrenia are that they are chronic, longer lasting, stable (i.e. symptoms don’t change frequently). It may also be that they are more bizarre and associated with incongruent moods, and are more disabling than other type of psychosis. Thus, it is important to rule out other possibilities before making a diagnosis of Schizophrenia.
-
Mood disorders and Psychosis: Extreme mood states like severe depression and mania are also associated with psychotic symptoms. While few patients with other illnesses like Borderline personality disorder may experience short lasting elation or euphoria in which they may experience ill-formed psychotic symptoms. This may be different from psychotic symptoms experienced in Mania (drastic shift in mood to irritable or euphoric mood which is disabling) or Hypomania (a less drastic shift in mood to irritable or euphoric mood which is less disabling). The psychotic symptoms associated with mood symptoms usually develop after the onset of mood symptoms and in the context of mood state e.g. in a depressed individual there may be delusion that they are getting poor even when they have enough resources; on the contrary a manic individual may have a delusion that they are a billionaire and make plans accordingly opposite to contrary. Treating the underlying mood episode and short-term use of antipsychotics is helpful.
-
Schizoaffective disorder: these are the disorders where one sees a combination of psychotic symptoms as well as mood symptoms. The distinguishing feature of schizoaffective disorders from the above two categories is that the mood symptoms and the psychotic symptoms exist independent of each other if we look at the long-term pattern of the illness. And there are periods of overlap between them.
-
Medical disorders and Psychosis: Medical issues like stroke, dementia, chemical changes in body salt like sodium/ potassium etc. may give rise to psychotic symptoms. The underlying changes vary from disease to disease but overall it is seen that the improvement in the underlying condition also improves the psychotics symptoms. In case there are any residual symptoms or the underlying medical problem is less likely to improve then a trial of antipsychotics may be given.
-
Stress and psychosis: Psychosis may occur within the context of lack of sleep, stress, extreme trauma etc. which is sometimes referred to as “psychotic breakdown”. This type of psychosis is shorter, lasting typically less than a month and rarely up to three months. Apart from psychotic symptoms a mixture of other symptoms may be seen e.g. emotional turmoil, anxiety, mood swings, irritability etc. These symptoms fluctuate in severity and nature from time to time throughout the course. Many individuals may also have these symptoms even without a stressor. In either case treatment should be taken at the earliest and any progression of symptoms beyond three months should be taken seriously.
The unconscious origin of psychosis.
Psychosis can be understood only when we take into account the existence of the unconscious mind. Without a belief in the unconscious we cannot understand psychosis. It is the unconscious that brings forth our dreams and it is outside the realms of time, space and rationality. The unconscious mind is the storehouse of all of our past experiences; joys, fears, worries, sadness, secrets etc. It is full of all the unpleasant aspects that we do not even want to admit to ourselves. It is also the storehouse of all the sublime and joyful experiences that one can experience in this lifetime. It is the unconscious that connects us to a larger universal mind from which it can draw both positive and negative thoughts.
The unconscious mind has a much larger capacity than the conscious mind but it is the conscious mind that keeps the unconscious in check. It is very much like the horse and the horseman where the horse represents the unconscious mind and the horseman the conscious mind. Normally the horseman is in full control of the horse, but in a psychotic state, it is the horse that takes over the horseman and takes him to places he may not want to go.
The symptoms of psychosis can be understood in terms of two broad categories:
-
Exaggeration of our own fears, denials, projections and suspicions. This first part of psychosis can be understood in terms of things that we have thought about in the past. These experiences get stored in the unconscious mind and come out when the barriers between the conscious and the unconscious are weakened. This part of the mind can be described as the personal unconscious i.e. a collection of our own past experiences.
-
Things that are totally bizarre and alien to us. This can be understood in terms of experiences coming from the collective unconscious, the part of mind that can also be described as the universal mind.
Recent insights into the causation of the illness shows that there can be a combination of biological, social psychological and genetic factors. In brain there can be an imbalance in the levels of naturally occurring brain chemicals or neurotransmitters DOPAMINE and GLUTAMATE or there may be an actual change in the brain structure from normal brain. These changes when interact with psychosocial stressors may precipitate the disease. The use of antipsychotics leads to a correction of dopamine overactivity.
Is psychosis a genetic disorder?
It is not a purely a genetic disorder but the chances of getting the disease increase in the future generation if one has suffered from it. In the case the psychosis, if it is due to more severe illness like schizophrenia, then chances increase by 1-10 % if either parent have the disease. But apart from genetics other factors like stress, illicit drugs, alcohol, and brain damage ,etc may precipitate the disease.
Are patients with psychosis violent?
Many people think that patients with psychosis are violent, which increases the stigma associated with the illness. The risk of violence in patients with psychosis is only two-fold higher than general population. Higher risk is associated with those who use substances. Patients with psychosis are more prone to be victims of violence than the perpetrators. Less than 10% patients diagnosed may be violent in their lifetime.
Is psychosis a part of Depression?
Psychosis may be associated with depression. There is a two-way relationship, i.e., depression may occur secondary to psychosis, and psychosis may occur secondarily after development of depressive disorder. In the context of psychosis, it is common to find depressive symptoms in the prodrome (i.e. before development of a full blown psychotic illness), during psychosis, or after resolution of psychotic symptoms once the individuals gain insight.
Is there a treatment for psychosis?
The treatment for psychosis is correcting the underlying disorder. In case it is due to a medical disorder, the improvement in psychosis occurs as the medical problem improves. If the problem is due to Alcohol, illicit drugs then stopping the use of the substance may help. Similarly the underlying psychiatric illness, if present, is to be treated. Antipsychotic drugs like Haloperidol, Olanzapine, Aripiprazole etc. may be given to help decrease the symptoms of psychosis and make thoughts clearer. Overall drugs support the recovery process and help in the process of natural healing of the underlying pathology. If the symptoms are due to stress and there are any unresolved issues then the client can benefit from psychotherapy.
The antipsychotics are divided into two broad categories: the first-generation and the second generation. The first generation are relatively older molecules e.g. Haloperidol, Trifluoperazine, and these drugs act specifically on dopaminergic areas of brain. Thus due to their highly specific action on dopamine they are associated with higher chances of side effects such as rigidity, tremor, abnormal movements, Parkinson like symptoms etc.
The second-generation antipsychotics such as Aripiprazole, Olanzapine etc. have a relatively less specific action on Dopamine thus the chances of movement related side effects are less. In addition to dopaminergic areas they also act on other brain areas like serotonin receptors, Glutamate receptors etc. But these drugs come with a higher risk of weight gain, obesity, change in lipid levels etc.
Overall, there is no evidence that second generation antipsychotics are clinically more effective better than first generation, and the decision of which is to be preferred in a given individual is taken after discussing the side effect profile of a given drug.
Where should I seek help from?
If you or your dear ones are having symptoms mentioned above with significant distress or problems in carrying normal activities, you should consult your psychiatrist immediately. The psychiatrist will evaluate thoroughly for the symptoms of psychosis, whether you require treatment or not and order any investigations if required.
The majority of patients improve with treatment of the underlying condition, and some would require drugs for their recovery.
After relevant examination, the decision to treat on out-patient or in-patient basis is taken. The cases where admission may be indicated are – if high there is a high suicidal risk, inability to take adequate self-care, danger to others, need for intensive therapy, or any medical/psychiatric complication.
Recommended Reading
- Psychosis – for young people | Royal College of Psychiatrists. RC PSYCH ROYAL COLLEGE OF PSYCHIATRISTS. Available from: https://www.rcpsych.ac.uk/mental-health/parents-and-young-people/young-people/psychosis—for-young-people
- Psychosis for parents and carers | Royal College of Psychiatrists. RC PSYCH ROYAL COLLEGE OF PSYCHIATRISTS. Available from: https://www.rcpsych.ac.uk/mental-health/parents-and-young-people/information-for-parents-and-carers/psychosis-information-for-parents-and-carers
